Mapping heart attack at AIIMS OPD: A sea of 20 to 50-year-olds
'Almost one-fourth of post-surgery patients go back with a heart pumping capacity of less than 35 per cent. They survive but they do so with a weakened heart. And this could have been avoided if they had identified symptoms and intervention had begun early,' says Dr Ambuj Roy, Professor of Cardiology
 They are an indicator of India’s rising burden of heart disease
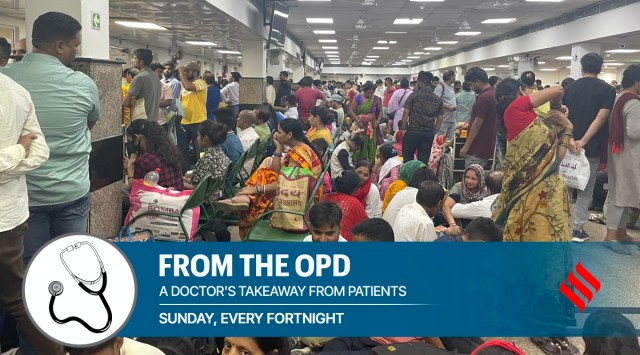
They are an indicator of India’s rising burden of heart disease 2 pm, Cardiothoracic and Neuro Centre OPD, AIIMS: Around 1,500 people are falling over each other, worry written large on their faces as they wonder if their doctors can see them. The AIIMS cardiac OPD runs three days a week with 10 consultants and 10 senior resident doctors but they are not enough to see all the patients who have queued up here. They are an indicator of India’s rising burden of heart disease as security guards categorise them into two sections: New patients and follow-ups. Most patients are between the ages of 20 and 50, living examples of what many studies have confirmed, that heart disease shows up in Indians a decade earlier than the rest of the world population. The younger lot seems to be pretty well aware of lifestyle modifications as they share notes on diet and fitness routines. Somebody says they have reduced their salt intake and given up packaged food altogether. Another says he has given up red meat for good. Yet another paces up and down the corridor to make up his daily quota of steps while waiting out his turn.
One of them is 36-year-old Manoj, a resident of Dakshinpuri, Delhi who has been visiting the AIIMS cardiology unit for the last two years. He had a heart attack after a bout of COVID-19. “One fine day I felt breathless and I came to the AIIMS emergency when I didn’t settle even with medication,” he says. He was diagnosed with an enlarged heart which can be caused by damage to the heart muscle or any condition that makes the heart pump harder than usual. Manoj, who has never had cigarette or alcohol in his life, except some stress and lack of sleep that are a part of any event manager’s job, didn’t see a heart attack coming.
He is being treated by Dr Ambuj Roy, professor of cardiology at AIIMS, who says his patient was quick to seek medical attention unlike most. “Often patients lose their lives because they cannot identify their symptoms on time. Our recent study showed that more than half of heart attack deaths happen at home because of delay in treatment. Everybody who has a heart attack obviously doesn’t die but because of the blockage in the artery, the muscle supplied by that particular artery dies. So you live with a weak heart because that scarred tissue is non-functional. The heart’s pumping mechanism becomes weak and ultimately these people develop congestion and heart failure. In fact, our registries show that almost one-fourth of post-surgery patients go back with a heart pumping capacity of less than 35 per cent. They survive but they do so with a weakened heart. And this could have been avoided if they had identified symptoms and intervention had begun early,” Dr Roy adds.
He sees around 25-30 new patients on OPD days and around 70 follow-up cases. Can the bulge in new cases be attributed to Covid? “More evidence is required to make any claim about a direct correlation. We have now stopped asking patients if they have had Covid because, as per all sero surveys, a majority of them have had it,” he says. But he does admit that the old troubles of the heart, which were due to malnutrition and valve shrinkage, have reduced and there are more cases of lifestyle-induced blockages. “Lack of exercise, unhealthy diet, lack of sleep and stress are posing a never before challenge to the body’s capacity and are resulting in a higher number of heart attacks,” says Dr Roy. And doctors have their hands full.




































